IMPROVING PATIENT HAND HYGIENE
Janeen McKeown
(Senior Infection Prevention & Control Nurse, BHSCT)
C.difficile causes significant morbidity and
mortality
We have tried to reduce C.difficile acquisition and
transmission using a variety of measures however
had not focused on patient hand hygiene before
There are many other benefits of improved
patient hand hygiene including improved general
hygiene, comfort and general sense of wellbeing
• It is very important to understand the processes within the
ward/department prior to commencing a quality
improvement project
• Good communication and team working are essential in
order for a project to succeed
• It is difficult to change behaviours!
• The information poster did not appear to alter behaviour
• Verbal and physical prompts appear to result in an
improvement (however, all staff did not implement 'the
change idea')
Meet with the team to review the progress to date
Plan a further PDSA cycle to 'add in' staff education
Liaise with other professionals, such as Occupational
Therapy, to determine what other strategies may be
appropriate
To share the learning in the fracture service and BHSCT
Why is this important?
The Results so far…
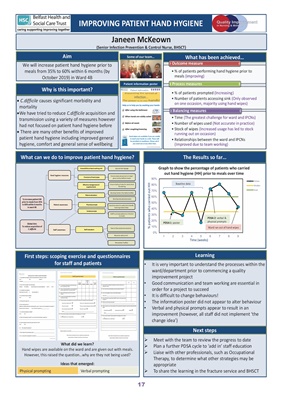
Aim
We will increase patient hand hygiene prior to
meals from 35% to 60% within 6 months (by
October 2019) in Ward 4B
What has been achieved…
What can we do to improve patient hand hygiene?
What did we learn?
Hand wipes are available on the ward and are given out with meals.
However, this raised the question…why are they not being used?
Ideas that emerged:
First steps: scoping exercise and questionnaires
for staff and patients
Physical prompting Verbal prompting
Learning
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
1 2 3 4 5 6 7 8 9
Graph to show the percentage of patients who carried
out hand hygiene (HH) prior to meals over time
Values
Median
Goal
Time (weeks)
% patients who carried out HH
Baseline data
PDSA 2: verbal &
physical prompts
PDSA 1: poster
Ward ran out of hand wipes
• % of patients performing hand hygiene prior to
meals (improving)
Outcome measure
• % of patients prompted (Increasing)
• Number of patients accessing sink (Only observed
on one occasion, majority using hand wipes)
Process measures
• Time (The greatest challenge for ward and IPCNs)
• Number of wipes used (Not accurate in practice)
• Stock of wipes (Increased usage has led to stock
running out on occasion)
• Relationships between the ward and IPCNs
(Improved due to team working)
Balancing measures
Next steps
Some of our team…
Patient information poster
17