and screening services (13).
Recommendations were made for each of
these areas with an urgent call for immediate
implementation of all of the recommendations
within five years. Effectively and efficiently
implemented, these recommendations could
prevent the huge toll of premature death,
disability and costs from cancer that
will otherwise be forthcoming (12).
Disappointingly, no significant changes have
occurred in these areas. Whatever activities
were implemented did not curb the advance of
cancer in the country, or at the most, were only
successful in few places mainly in Metro
Manila.
The My Child Matters programme at
PCMC
A demonstration project was implemented at
the Philippine Children's Medical Center
(PCMC) in 2006, as part of the Sanofi Espoir
Foundation and UICC My Child Matters
(MCM) programme, and in partnership with
the International Network for Cancer
Treatment and Research (INCTR). The goal was to create
public awareness about the curability of childhood cancer,
particularly childhood leukaemia, and implement
community mobilization campaigns. It focused public
attention to address delays in diagnosis and high treatment
abandonment rates that were mainly responsible for poor
survival rates of childhood cancer in the Philippines
postulated to be at 10% (14). The ultimate objective was to
improve survival rates of leukaemia, the most common type
of childhood cancer in the Philippines, to at least 50% in five
years. The strategy was to: 1) train frontline physicians in
early cancer detection; 2) develop capabilities for satellite
treatment units outside of Metro Manila; and 3) address
affordability issues of chemotherapy mainly responsible for
high treatment abandonment rates.
Consequently, during the last ten years, PCMC mobilized
stakeholders for a national public awareness campaign
targeting early detection and effective treatment of
childhood cancer. First, using a network of alumni from two
paediatric oncology training centres (i.e. PCMC and the
Philippine General Hospital), an initial referral network of 13
hospitals in five regional catchment areas was established.
These paediatric oncologists led activities aimed at
increasing early detection. Partnership with the tri-media
was forged for a massive national public awareness
REGIONAL INITIATIVES
140 CANCER CONTROL 2015
campaign. As a result, late stage diagnosis decreased to 30%
from 70% when patients are seen for the first time in these
hospitals.
The PCMC Cancer Center
In 2008, the Department of Health (DoH) designated PCMC
as the national end-referral cancer centre for children, later
providing funds thereof for the construction of a cancer
centre facility. PCMC renovated an existing ward to
establish quickly an operational Pediatric Cancer and
Hematology Center which was launched in 2010. In 2011,
the DoH's National Center for Pharmaceutical Access and
Management (NCPAM) partnered with PCMC and MCM in
the implementation of its Acute Lymphoblastic Leukemia
Medicines Access Program (ALLMAP), which provided for
free chemotherapy drugs to indigent patients, funds for the
establishment of a data registry, and for the training of
health-care professionals directly involved in childhood
cancer management. In June 2012, the participating
hospitals in the MCM referral network expanded to 24
government and privately-owned hospitals from the original
13, which are now all recipients of the NCPAM's ALLMAP.
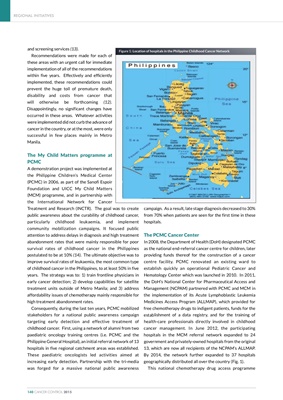
By 2014, the network further expanded to 37 hospitals
geographically distributed all over the country (Fig. 1).
This national chemotherapy drug access programme
Figure 1: Location of hospitals in the Philippine Childhood Cancer Network