services, or can do so only with limited and often inadequate
resources. Access to care will therefore be a great challenge
to majority of patients.
Within ten years of the MCM programme, national public
awareness campaigns brought down the number of late
diagnoses to 30%-40% from a baseline of 70% (16). The
current national referral and treatment network of 39
paediatric oncologists in 37 hospitals made subspecialty
care nationally available, particularly to poorer patients
outside of Metro Manila, reaching an annual average of
2,553 patient beneficiaries to date from a baseline of only
about 1,000 (16). Treatment abandonment rate was brought
down to 10%-20% from a baseline of 80%, and the currently
available survival rate for childhood leukaemia based on
hospital-based data from participating hospitals improved to
78% from a baseline of only 16%-20% (16). To further
expand services to as many places in the country without
paediatric oncologists, PCMC has now increased the
number of clinical fellows entering first year in the training
programme to four from an initial of two, which together
with one from the UP-PGH are expected to provide in the
next ten years for an adequate number necessary for the
manpower need of the country for paediatric oncologists
who will practice in underserved areas outside the major
cities.
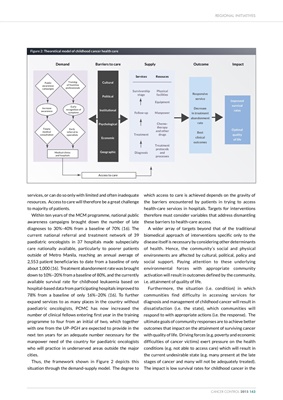
Thus, the framework shown in Figure 2 depicts this
situation through the demand-supply model. The degree to
which access to care is achieved depends on the gravity of
the barriers encountered by patients in trying to access
health-care services in hospitals. Targets for interventions
therefore must consider variables that address dismantling
these barriers to health-care access.
A wider array of targets beyond that of the traditional
biomedical approach of interventions specific only to the
disease itself is necessary by considering other determinants
of health. Hence, the community's social and physical
environments are affected by cultural, political, policy and
social support. Paying attention to these underlying
environmental forces with appropriate community
activation will result in outcomes defined by the community,
i.e. attainment of quality of life.
Furthermore, the situation (i.e. condition) in which
communities find difficulty in accessing services for
diagnosis and management of childhood cancer will result in
dissatisfaction (i.e. the state), which communities will
respond to with appropriate actions (i.e. the response). The
ultimate goals of community responses are to achieve better
outcomes that impact on the attainment of surviving cancer
with quality of life. Driving forces (e.g. poverty and economic
difficulties of cancer victims) exert pressure on the health
conditions (e.g. not able to access care) which will result in
the current undesirable state (e.g. many present at the late
stages of cancer and many will not be adequately treated).
The impact is low survival rates for childhood cancer in the
REGIONAL INITIATIVES
CANCER CONTROL 2015 143
Public
awareness
campaigns Demand
Training
of frontline
professionals
Timely
medical
consultation
Early
referral to
specialists
Increase
awareness
Early
recognition of
symptons
Medical clinics
and hospitals
Barriers to care Supply Outcome Impact
Access to care
Cultural
Political
Institutional
Psychological
Economic
Geographic
Services
Survivorship
stage
Follow-up
Treatment
Diagnosis
Resouces
Physical
facilities
Equipment
Manpower
Chemotherapy
and other
drugs
Treatment
protocols
and
processes
Improved
survival
rates
Optimal
quality
of life
Responsive
service
Decrease
in treatment
abandonment
rate
Best
clinical
outcomes
Figure 2: Theoretical model of childhood cancer health care