these issues are, or have been partially addressed (e.g., half
price bus tickets for cancer patients and free treatment for
children less than five-years old in Tanzania), such funds must
come from the government and are not always available.
Even if families overcome these obstacles, they face the
challenge of extremely limited numbers of nurses, doctors
and pharmacists, and remarkably few cancer specialists
(Tanzania has, for example, a single trained medical
oncologist, no trained paediatric oncologist, two or three
radiation oncologists and perhaps 18 pathologists, almost all
working in major cities).
Access to specialist health services
Unlike other non-communicable diseases, some patients
with cancer are curable through access to earlier and more
accurate diagnosis, specialist consultation and therapy.
Drugs vary markedly in price, even within the same country,
and may sometimes be higher than in the United States or
Europe. This precludes many regimens since most patients
must generally pay out-of-pocket for all diagnostic and
treatment costs. To address this situation, the methods of
education, the division of labour and the delivery of health
services, including cancer services, will need to be markedly
improved. Considerations include:
‰ enactment of equitable policies to subsidize the costs of
care e.g., universal health care;
‰ insurance schemes;
‰ diagnostic and therapeutic co-pay;
‰ increased practical responsibility for medical assistants,
nurses and community health workers;
‰ shortening of training periods for health professionals;
‰ incentivization for practice in rural regions e.g. locating
medical and nursing schools in rural regions, required
rural service periods for health professionals and rural
living subsidies;
‰ re-focusing and re-balancing the mix of academic
(degree-based), discipline/competency-based training
(professional certification) and practical service
delivery.
Medical professional migration
Higher-resourced countries recruit extensively from lesserresourced nations despite these countries having
major
shortages of health workers.3 Concomitantly, although not at
a high level of development, some countries (e.g., India) have
well-equipped and staffed hospitals, generally in the private
sector, that are able to attract patients from high resource
countries for surgical procedures or to provide services such
as interpretations of electronically-transmitted images
(radiographs, etc.). Accordingly, an additional proportion of
the skilled health care providers, already too few to meet
national needs, are lost to their own country. The least
developed countries cannot compete in this market, although
many African doctors choose to work (sometimes to train and
work) in countries with higher levels of development. The
solution is to improve the overall level of care in regions such
as East Africa. This process will proceed much more rapidly
when external educators spend time in countries with
limited development, or at least assist them through
teleconferences, etc. Institution-to-institution collaborations
("twinning") between a high-resource and lesser-resourced
country can be of great value (see article by Raul
Ribeiro), However, international institution-to-institution
programmes are unlikely to promote the building of networks
required to strengthen services across health sectors.
Cancer treatment: Shared care among specialists
and hospitals
Drugs and equipment are of no value without knowledgeable
health professionals, particularly oncologists who can make
treatment decisions and work with a team comprised of
pharmacists, oncology nurses, junior doctors, medical
assistants and social workers. Unfortunately, it can be
difficult or impossible to create such teams when there is no
oncologist to take a leading role. An European Society for
Medical Oncologists survey (2006) reported that only 22
countries of the 39 respondents were able to state how many
oncologists there were in the country and of those who could
provide figures, the number of oncologists per million cancer
CANCER MANAGEMENT
CANCER CONTROL 2014 61
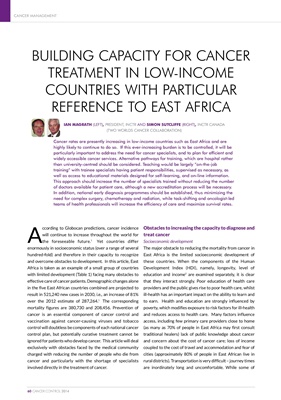
Table 1: UNDP HDI, 2012
Burundi Rwanda Uganda Tanzania Kenya
HDI 0.355 0.434 0.456 0.476 0.519
Rank 178 167 161 152 145
GDP (Current US$, billions) 2.47 7.10 20.03 28.24 40.70
Physicians per 1,000 people ND 0.1 0.1 0.1 0.2
HDI maximum score, 1. Norway's HDI was 0.921 in 2012; GDP figures are for 2012 - UK GDP = 2,476 trillion; UK physicians per 1,000 people = 2.7 (2010/2011); ND = No data